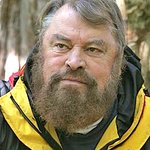
An open letter spearheaded by Animal Defenders International (ADI) and signed by nearly 100 experts, academics, and other concerned parties including Brian Blessed, Jenny Seagrove, Alexei Sayle and Benjamin Zephaniah, is calling for advanced non-animal research methods to be prioritised to accelerate the discovery and use of effective vaccines and treatments for COVID-19.
Published ahead of the World Health Assembly on Monday 18 May, and directed at the World Health Organization, governments, funding bodies, and regulators, the letter states that “significant funding and precious time is being spent on animal research…. despite the known species differences which make the results from such data unreliable when translated to humans.”
The open letter can be viewed here.
Signatories include Dr Laura Leslie, a biomedical engineer at Aston University working on human airways models; respiratory medicines specialist Dr Aryan Tavakkoli; Professor Jon Heylings, Chairman and Owner of Dermal Technology Laboratory Ltd and Professor of Toxicology at Keele University; Dr Malcom Wilkinson, Managing Director at Technology For Industry Ltd; Professor Alberto Alemanno, Professor of EU Law; Professor Marc Bekoff, Professor Emeritus of Ecology and Evolutionary Biology at University of Colorado; Dr Simon Brooman, Senior Lecturer in Animal Law at Liverpool John Moores University; Dr Charlotte E Blattner, Doctor of Animal Law at Harvard Law School; and Kirstall Ltd.
“Since the identification of SARS-COV-2, the virus which causes COVID-19, there has been a surge in funding of research and testing to find a vaccine and treatments, with unprecedented collaboration and openness between researchers worldwide.” the letter states.
Vaccine research and development typically takes 15-20 years, with animal research, currently, a major part of the process. There are however reports that a vaccine for the virus could be available from as early as next year.
In a move to accelerate the process, the International Coalition of Medicines Regulatory Authorities (ICMRA) has advised that the usual animal disease models to test the effectiveness (efficacy) of potential vaccines for the virus are not required before proceeding to human clinical trials. Despite this, such tests are still taking place, and in some cases in parallel with clinical trials.
Although efficacy tests using animals do not need to be undertaken, before a potential vaccine can be put on the market, safety testing – for which animals will typically be force-fed or injected with a substance while restrained, and suffer debilitating, even fatal, side effects – will still be required.
Due to species differences, animals respond differently to substances such as drugs, and are therefore an unreliable way to predict effects in humans. More than 90% of drugs which prove promising in animal trials fail in humans, either due to lack of effectiveness or safety concerns.
Despite this recognised, fundamental problem, laboratories around the world, including in the UK, US, Netherlands, and China, are using animals to test possible vaccines for COVID-19.
“Mice are one of the most commonly used species in drug and vaccine research” the open letter states and "in addition to major differences between human and mouse respiratory systems, species differences specific to research for SARS-COV-2 include that mice do not naturally have the same receptors the virus uses to infect human cells. Researchers are now attempting to “humanize” mice to ensure they contract the virus. Such fundamental differences risk impeding the production of vaccines and other treatments to help prevent and reduce the symptoms of COVID-19 in people."
“While time, resources and efforts are being put into attempting to find the “ideal” animal model, advanced non-animal scientific methods, which relate directly to the disease in humans, are being progressed. These sophisticated research methods have the potential to deliver safer, more effective vaccines and treatments to the market more quickly but need more funding and support. Advanced techniques include mathematical modelling of transmission and size of the epidemic; the use of patient lung fluid cultures to study the virus genome; patient biopsy samples to investigate lung tissue damage; artificial intelligence models to predict which drugs could treat COVID-19; using antibodies from COVID-19 survivors to treat patients; human organ-on-a-chip technology emulating human lung infection for drug discovery; organoids to investigate how the disease infects human tissue; and in vitro 3D human airway cell models for evaluating drugs."
Over 51,000 people have supported, to date, a new ADI petition calling for animal tests to be cut to tackle COVID-19. Sign the petition here.
ADI President Jan Creamer: “There is an urgent need to tackle and treat COVID-19 and other human disease with better, faster science. To provide safer, more effective treatments to help people, we need to move away from unreliable animal research and use advanced scientific methods, more relevant to humans.”
“The respiratory systems of animals used for COVID-19 research are known to be different from ours physiologically, so it is only logical that human-based methods be prioritised and used for testing treatments and vaccines.” says Dr Aryan Tavakkoli MRCP FRACP, Respiratory Physician. “With incredibly sophisticated methods such as human lung models available, it is vital that resources and time are directed toward these to find treatments and a vaccine for this life-threatening virus.”